Have a new insurance plan? Make sure your SKYRIZI is covered.



Discover SKYRIZI savings
You could get SKYRIZI for as little as $0* per dose
Skyrizi Complete can help you save on your prescribed treatment:
- If you’re eligible for the Skyrizi Complete Savings Card, you may pay as little as $0 per dose
- Prescription rebates could also help eligible, commercially insured patients save on out-of-pocket costs
- If you have government insurance or are not insured, there may be other affordable options
Haven’t signed up for Skyrizi Complete?
*For eligible, commercially insured patients only. See Terms and Conditions. $0 per dose for SKYRIZI.
Use the Complete App to access your Savings Card
That way, you're always ready when it's time to pay for your prescription.
Download the App
Search for “Complete App” at the App Store® or Google Play™.
Or text APP to 29279 to receive a link to download the app.
Message and data rates may apply. By texting APP to 29279, you agree to AbbVie’s Terms and Conditions and Privacy Notice.

See how Skyrizi Complete can help you find potential ways to save
SUPER/ANNOUNCER 1 VOICEOVER (V.O.):
Please see Important Safety Information near the end of this video.
Please see link for the full Prescribing Information, including the Medication Guide, for SKYRIZI.
USES1
SKYRIZI is a prescription medicine used to treat adults with:
- moderate to severe plaque psoriasis who may benefit from taking injections or pills (systemic therapy) or treatment using ultraviolet or UV light (phototherapy).
- active psoriatic arthritis.
- moderate to severe Crohn's disease.
- moderate to severe ulcerative colitis.
SAFETY CONSIDERATIONS1
Do not use if you are allergic to SKYRIZI. SKYRIZI may cause serious side effects, including serious allergic reactions, an increased risk of infections, and liver problems.
- Stop using SKYRIZI and get emergency medical help right away if experiencing symptoms of a serious allergic reaction.
- Before starting treatment, your doctor should check for infections and tuberculosis. Tell your doctor right away about any infections or symptoms of infection and about planned or recent vaccines.
- Liver problems may happen while being treated for Crohn's disease or ulcerative colitis that can lead to hospitalization. Your doctor will do liver blood tests before and during treatment and may stop SKYRIZI if liver problems develop.
SUPER/ANNOUNCER 2 V.O.:
IS IT POSSIBLE TO LOWER MY COST FOR SKYRIZI?
PATIENT V.O.:
When I was prescribed SKYRIZI, I wasn't totally sure what my co-pay and other costs would be. So I called Skyrizi Complete, and they connected me to an Insurance Specialist.
SUPER:
Insurance Specialist
1.866.SKYRIZI
PATIENT V.O.:
Since I have commercial insurance, they explained how I could get this Savings Card to help lower my out-of-pocket costs to as little as $0 a dose.
SUPER:
As little as $0 PER DOSE
*For eligible, commercially insured patients only. See Terms and Conditions at the end of this video.
SUPER/ANNOUNCER 2 V.O.:
HOW DOES THE SKYRIZI COMPLETE SAVINGS CARD WORK?
PATIENT V.O.:
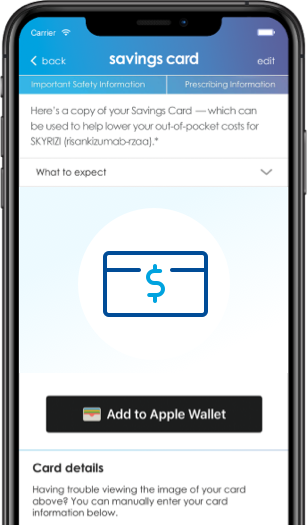
Okay so, after I signed up for Skyrizi Complete, I requested a Savings Card on the Skyrizi Complete App. When the Specialty Pharmacy calls to process my prescription, I read them the number on the card.
SUPER:
Download the Skyrizi Complete App now. Open the App Store or Google Play and search "Skyrizi Complete".
Specialty Pharmacy
PATIENT V.O.:
And if there's an issue using your card, an Insurance Specialist can work with your Specialty Pharmacy to make sure your savings go through.
SUPER:
HOW TO REQUEST A SKYRIZI COMPLETE SAVINGS CARD:
- SkyriziCompleteSavings.com
- The Complete App
- Talk to an Insurance Specialist
Download the Skyrizi Complete App now. Open the App Store or Google Play and search "SKYRIZI Complete."
PATIENT V.O.:
If you don't have a Savings Card yet, you can request one online or through the Complete App. And you can access it at any time.
Or just ask an Insurance Specialist—they can help you get one. And if you're not eligible, they may be able to help find other options that could lower the cost you pay for SKYRIZI, too.
SUPER/ANNOUNCER 2 V.O.:
CAN I STILL SAVE IF I DON'T HAVE A SAVINGS CARD?
PATIENT V.O.:
Well, if you don't have a Savings Card or aren't able to use it, prescription rebates may be an option. Take a look at the Complete site or the App to find out about it.
SUPER:
Save with rebates
Submit rebates:
- On the Skyrizi Complete site
- Through the Complete App
- By mail
PATIENT V.O.:
Look, sometimes things come up that can affect insurance. Like if I lost my job or my coverage changed. I can always call an Insurance Specialist. They may be able to help find other ways to save.
SUPER:
Uninsured
You may qualify for myAbbVie Assist
PATIENT V.O.:
So call an Insurance Specialist to see what you qualify for. They're good about trying to make SKYRIZI affordable. That's what I did and they were so helpful.
SUPER:
YOU GOT THIS
HERE ARE THE STEPS YOU CAN TAKE RIGHT NOW:
- Call Skyrizi Complete for an Insurance Specialist.
- Have them look up your current out-of-pocket costs
- Request a Skyrizi Complete Savings Card
- Give your Savings Card info when filling your prescription
- Ask the Specialist about other savings options
PATIENT V.O.:
Don't forget that there are a few things that you can do right now: Call Skyrizi Complete and ask for an Insurance Specialist. Have them look up your out-of-pocket costs. Then you're gonna request a Savings Card. And remember to use that card each time you fill your prescription. And if you're unable to get a card, ask the Insurance Specialist about the other savings options that may be available.
SUPER:
FOR HELP FINDING WAYS TO SAVE ON SKYRIZI, CALL 1.866.SKYRIZI (1.866.759.7494) AND SPEAK WITH AN INSURANCE SPECIALIST.
Chat with us live 24/7 at SkyriziComplete.com
PATIENT V.O.:
Just give Skyrizi Complete a call at 1.866.SKYRIZI and speak with an Insurance Specialist.
SUPER/ANNOUNCER 1 V.O.:
IMPORTANT SAFETY INFORMATION1
What is the most important information I should know about SKYRIZI® (risankizumab-rzaa)?
SKYRIZI is a prescription medicine that may cause serious side effects, including:
Serious allergic reactions:
- Stop using SKYRIZI and get emergency medical help right away if you get any of the following symptoms of a serious allergic reaction:
- fainting, dizziness, feeling lightheaded (low blood pressure)
- swelling of your face, eyelids, lips, mouth, tongue, or throat
- trouble breathing or throat tightness
- chest tightness
- skin rash, hives
- itching
Infections:
SKYRIZI may lower the ability of your immune system to fight infections and may increase your risk of infections. Your healthcare provider should check you for infections and tuberculosis (TB) before starting treatment with SKYRIZI and may treat you for TB before you begin treatment with SKYRIZI if you have a history of TB or have active TB. Your healthcare provider should watch you closely for signs and symptoms of TB during and after treatment with SKYRIZI.
- Tell your healthcare provider right away if you have an infection or have symptoms of an infection, including:
- fever, sweats, or chills
- cough
- shortness of breath
- blood in your mucus (phlegm)
- warm, red, or painful skin or sores on your body different from your psoriasis
- weight loss
- diarrhea or stomach pain
- burning when you urinate or urinating more often than normal
Do not use SKYRIZI if you are allergic to risankizumab-rzaa or any of the ingredients in SKYRIZI. See the Medication Guide or Consumer Brief Summary for a complete list of ingredients.
Before using SKYRIZI, tell your healthcare provider about all of your medical conditions, including if you:
- have any of the conditions or symptoms listed in the section "What is the most important information I should know about SKYRIZI?"
- have an infection that does not go away or that keeps coming back.
- have TB or have been in close contact with someone with TB.
- have recently received or are scheduled to receive an immunization (vaccine). Medicines that interact with the immune system may increase your risk of getting an infection after receiving live vaccines. You should avoid receiving live vaccines right before, during, or right after treatment with SKYRIZI. Tell your healthcare provider that you are taking SKYRIZI before receiving a vaccine.
- are pregnant or plan to become pregnant. It is not known if SKYRIZI can harm your unborn baby.
- are breastfeeding or plan to breastfeed. It is not known if SKYRIZI passes into your breast milk.
- become pregnant while taking SKYRIZI. You are encouraged to enroll in the Pregnancy Registry, which is used to collect information about the health of you and your baby. Talk to your healthcare provider or call 1-877-302-2161 to enroll in this registry.
Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements.
What are the possible side effects of SKYRIZI?
SKYRIZI may cause serious side effects. See "What is the most important information I should know about SKYRIZI?"
Liver problems may happen while being treated for Crohn's disease or ulcerative colitis: A person with Crohn's disease who received SKYRIZI through a vein in the arm developed changes in liver blood tests with a rash that led to hospitalization. Your healthcare provider will do blood tests to check your liver before, during, and at least up to 12 weeks of treatment, and may stop treatment with SKYRIZI if you develop liver problems. Tell your healthcare provider right away if you notice any of the following symptoms: unexplained rash, nausea, vomiting, stomach (abdominal) pain, tiredness (fatigue), loss of appetite, yellowing of the skin and eyes (jaundice), and dark urine.
The most common side effects of SKYRIZI in people treated for Crohn's disease and ulcerative colitis include: upper respiratory infections, headache, joint pain, stomach (abdominal) pain, injection site reactions, low red blood cells (anemia), fever, back pain, urinary tract infection, and rash.
The most common side effects of SKYRIZI in people treated for plaque psoriasis and psoriatic arthritis include: upper respiratory infections, headache, feeling tired, injection site reactions, and fungal skin infections.
These are not all the possible side effects of SKYRIZI. Call your doctor for medical advice about
side effects.
Use SKYRIZI exactly as your healthcare provider tells you to use it.
SKYRIZI (risankizumab-rzaa) is available in a 150 mg/mL prefilled syringe and pen, a 600 mg/10 mL vial for intravenous infusion, and a 180 mg/1.2 mL or 360 mg/2.4 mL single-dose prefilled cartridge with on-body injector.
You are encouraged to report negative side effects of prescription drugs to the FDA. Visit www.fda.gov/medwatch or call 1-800-FDA-1088.
If you are having difficulty paying for your medicine, AbbVie may be able to help. Visit AbbVie.com/PatientAccessSupport to learn more.
SUPER:
Reference: 1. SKYRIZI [package insert]. North Chicago, IL: AbbVie Inc.
Skyrizi Complete Savings Card Terms & Conditions
Eligibility: Available to patients with commercial insurance coverage for SKYRIZI® (risankizumab-rzaa) who meet eligibility criteria. This co-pay assistance program is not available to patients receiving prescription reimbursement under any federal, state, or government-funded insurance programs (for example, Medicare [including Part D], Medicare Advantage, Medigap, Medicaid, TRICARE, Department of Defense, or Veterans Affairs programs) or where prohibited by law. Offer subject to change or termination without notice. Restrictions, including monthly maximums, may apply. This is not health insurance. For full Terms and Conditions, visit SKYRIZISavingsCard.com or call 1.866.SKYRIZI for additional information. For full Terms and Conditions for SKYRIZI Crohn's Disease and Ulcerative Colitis patients, visit www.skyrizi.com/savings-card-terms or call 1.866.SKYRIZI for additional information. To learn about AbbVie’s privacy practices and your privacy choices, visit https://abbv.ie/corpprivacy
Please see link for the full Prescribing Information, including the Medication Guide, for SKYRIZI.
©2024 AbbVie. All rights reserved. SKYRIZI® and its design are registered trademarks of AbbVie Biotechnology Ltd.
US-SKZ-240211
Using your Skyrizi Complete Savings Card
Here’s what you can expect:

Your specialty pharmacy will call you to coordinate payment and delivery of your SKYRIZI. If you do not receive a call, you can call them to start the process. Your doctor can help you confirm the pharmacy’s contact information if needed.

Provide the requested information from your Savings Card to receive savings on the cost of your prescription.
- First, provide your specialty pharmacy with your Rx ID, Rx Bin, Rx Group, and Rx PCN numbers from your Savings Card.
- If there is a remaining balance after using the Rx numbers on your card, your specialty pharmacy will contact you for additional card information.

Confirm the address where you would like SKYRIZI delivered.
Your Skyrizi Complete Nurse Ambassador† and Insurance Specialist can also help. Just call 1.866.SKYRIZI (1.866.759.7494).
†Nurse Ambassadors are provided by AbbVie and do not work under the direction of your health care professional (HCP) or give medical advice. They are trained to direct patients to their HCP for treatment-related advice, including further referrals.
Prescription rebates* may be an option
Eligible, commercially insured patients can be reimbursed for out-of-pocket costs for prescriptions.

A Skyrizi Complete Insurance Specialist to help navigate your unique situation
Regardless of your healthcare coverage, your Insurance Specialist will help you review all coverage options, understand details, and identify potential ways you may be able to save.
Just call 1.866.SKYRIZI (1.866.759.7494) to speak with an Insurance Specialist.
Other potential ways to save
People on Medicare who need help paying for their prescriptions may be eligible to receive a low-income subsidy (also known as Extra Help).
What is Extra Help?
Extra Help is a government program that helps pay the cost of your prescriptions beyond what your plan already covers. Eligibility is determined by the Medicare program based upon your income and resources.
Are you eligible for Extra Help?
Some people qualify automatically for Extra Help, while others need to apply—which means you may qualify.
3 ways to apply:
- Online at www.socialsecurity.gov/i1020
- Call Social Security at 1.800.772.1213 (TTY 1.800.325.0778)
- At your local State Medical Assistance (Medicaid) office
If you’re not eligible for Extra Help, SKYRIZI may still be available at no additional cost. Call 1.866.SKYRIZI (1.866.759.7494) to speak to an Insurance Specialist to learn more.
For more information on SKYRIZI and Medicare, go to Understanding Your Insurance ▸

Check out the “Understanding Medicare” brochure to learn more about what Medicare is, what it covers, and how it works.
If you are having difficulty paying for your medicine, AbbVie may be able to help. Visit AbbVie.com/PatientAccessSupport to learn more.
Frequently Asked Questions
The amount you pay for SKYRIZI can depend on a number of factors, including your access to prescription drug coverage, the type of insurance you have, and even the level of coverage your insurance may provide. To find out more, visit the SKYRIZI cost and savings page.
If you have a new insurance plan, does it cover SKYRIZI?
This checklist can help you make sure.
Check if you're covered in 2021

Live Chat Support
If you have questions or want to talk to a nurse, click the “Chat Live 24/7” button.
Skyrizi Complete Savings Card Terms & Conditions
Terms and Conditions apply. This benefit covers SKYRIZI® (risankizumab-rzaa) alone or, for psoriatic arthritis patients, SKYRIZI plus one of the following medications: methotrexate, leflunomide, or hydroxychloroquine. Eligibility: Benefit also covers certain lab tests to monitor for specific parameters as recommended in the product label where the full cost is not covered by patients’ insurance (Maximum savings limit of $1,000.00 per year applies). Available to patients with commercial insurance coverage for SKYRIZI who meet eligibility criteria. Co-pay assistance program is not available to patients receiving reimbursement under any federal, state, or government-funded insurance programs (for example, Medicare [including Part D], Medicare Advantage, Medigap, Medicaid, TRICARE, Department of Defense, or Veterans Affairs programs) or where prohibited by law or by the patient’s health insurance provider. If at any time a patient begins receiving prescription drug coverage under any such federal, state, or government-funded healthcare program, patient will no longer be able to use the Skyrizi Complete Savings Card and patient must call Skyrizi Complete at 1.866.SKYRIZI to stop participation. By enrolling in the co-pay assistance program, you agree that this program is intended solely for the benefit of you, the patient. Some health plans have established programs referred to as “accumulator adjustment” or “copay maximizer” programs. An accumulator adjustment program is one in which payments made by you that are subsidized by manufacturer assistance do not count toward your deductibles and other out-of-pocket cost sharing limitations. Co-pay maximizers are programs in which the amount of your out-of-pocket costs is increased to reflect the availability of support offered by a manufacturer assistance program. Except where prohibited by applicable state law, if your insurance company or health plan implements either an accumulator adjustment or co-pay maximizer program, you will not be eligible for, and agree not to use, co-pay assistance because these programs are inconsistent with our agreed intent that this program is solely for your benefit. You also agree that you are personally responsible for paying any amount of co-pay required after the savings card is applied. Any out-of-pocket costs remaining after the application of the savings card may not be paid by your health plan, pharmacy benefit programs, or any other program. If you learn your insurance company or health plan has implemented either an accumulator adjustment program or a co-pay maximizer program, you agree to inform AbbVie of this fact by calling 1.866.SKYRIZI to discuss alternative options that may be available to support you. Since you may be unaware whether you are subject to a co-pay maximizer program when you enroll in the co-pay assistance program, AbbVie will monitor program utilization data and reserves the right to discontinue co-pay assistance at any time if AbbVie determines that you are subject to a copay maximizer program. For such patients, except where prohibited by applicable state law, AbbVie may discontinue the availability of co-pay support at an amount not to exceed $4,000.00. This amount is subject to change without notice. If your health plan removes SKYRIZI from a co-pay maximizer program, you will return to eligibility for co-pay assistance up to the maximum annual benefit listed below. Subject to all other terms and conditions, the maximum annual benefit that may be available solely for the patient’s benefit under the co-pay assistance program is $14,000 per calendar year. The actual application and use of the benefit available under the co-pay assistance program may vary on a monthly, quarterly, and/or annual basis depending on each individual patient’s plan of insurance and other prescription drug costs. This co-pay assistance program is subject to change, reduction in monetary amount, or discontinuation without any notice. AbbVie in its sole discretion may unilaterally reduce or discontinue the maximum annual benefit for any reason. Except where prohibited by applicable law, this includes potential reduction or discontinuation to ensure that co-pay assistance is utilized solely for the patient’s benefit. Patients may not seek reimbursement for value received from the Skyrizi Complete Program from any third-party payers. Offer subject to change or discontinuance without notice. Restrictions, including monthly maximums, may apply. This assistance offer is not health insurance. By utilizing this co-pay assistance program, you hereby accept and agree to abide by these terms and conditions. Any individual or entity who enrolls or assists in the enrollment of a patient in the co-pay assistance program represents that the patient meets the eligibility criteria and other requirements described herein. Further, you agree that you currently meet the eligibility criteria and other requirements described herein every time you use the co-pay assistance program. To learn about AbbVie’s privacy practices and your privacy choices, visit https://abbv.ie/corpprivacy.
This Copay Assistance Card is issued by Florida Capital Bank pursuant to a license from Mastercard International. Serviced by Transcard LLC. The funds available through use of this Copay Assistance Card are not your property but are supplied exclusively by AbbVie Inc. No balance on this Copay Assistance Card is redeemable for cash or credit in the form of a refund, credit, change, or otherwise. This Copay Assistance Card may only be used for prescription medication at participating pharmacies and other approved locations, and for the specific purpose(s) expressly authorized by AbbVie Inc. Terms of Use, as amended from time to time. For a copy of the Terms of Use, please visit SKYRIZISavingsCard.com. For customer service questions or to report your Card lost or stolen, call 888-857-0636.